The Beginning: When a Parent’s Instinct Knows Something is Wrong
The diagnostic odyssey rarely begins with a dramatic event. It starts with a quiet, persistent whisper in the back of a parent’s mind. It’s a feeling, a gut instinct, that something is not quite right. It might be the subtle clumsiness that other people dismiss, the slight delay in speech that the pediatrician says is “within the normal range,” or the new, fleeting eye movements that no one else seems to notice. This is the power and the burden of parental instinct—the innate, profound connection that allows you to sense a deviation from your child’s unique baseline long before it shows up on any standard developmental chart.
In this first stage, you begin to question yourself. Are you overreacting? Are you just an anxious parent? Friends and family may offer reassurance, telling you that all kids develop differently. Yet, the whisper persists. This is the lonely, confusing start to a journey that will test your resilience, your marriage, your faith in the medical system, and every ounce of strength you possess. It is the beginning of your transformation from parent to relentless medical detective.
The Wilderness Years: Navigating Dismissal and Misdiagnosis
The next phase of the odyssey can feel like wandering in a vast, frustrating wilderness. You enter the complex world of the navigating the healthcare system, armed with your list of concerns. You start with your pediatrician, who may run some basic tests that come back normal. They refer you to a specialist—perhaps a neurologist, an ophthalmologist, or a developmental pediatrician. Each specialist looks at your child through the narrow lens of their own expertise.
The ophthalmologist might diagnose a retinal issue. The neurologist might diagnose a benign seizure disorder. Each specialist offers a piece of the puzzle, but no one steps back to see that the pieces don’t fit together to form a coherent picture. This period is often marked by a string of disconnected diagnoses and treatments that don’t work, all while your child may be slowly, almost imperceptibly, losing skills.
The Cycle of Specialists and “Normal” Test Results
You find yourself in a draining cycle of appointments, referrals, and tests. Blood work, EEGs, and initial brain scans may all come back within normal limits, further fueling your self-doubt. With each “normal” result, you can feel the doctor’s confidence in your concerns waning. This is where many families begin to experience a painful phenomenon that feels like medical gaslighting.
Your valid concerns are downplayed, your detailed observations are dismissed as anecdotal, and you may even be labeled as an Syndromes The implicit message is that the problem is not with your child, but with your perception. This is an incredibly damaging experience, as it erodes your confidence and makes you question your own sanity, even as your parental instinct screams that the search must continue.
The Turning Point: Finding the Right Clues and the Right Doctor
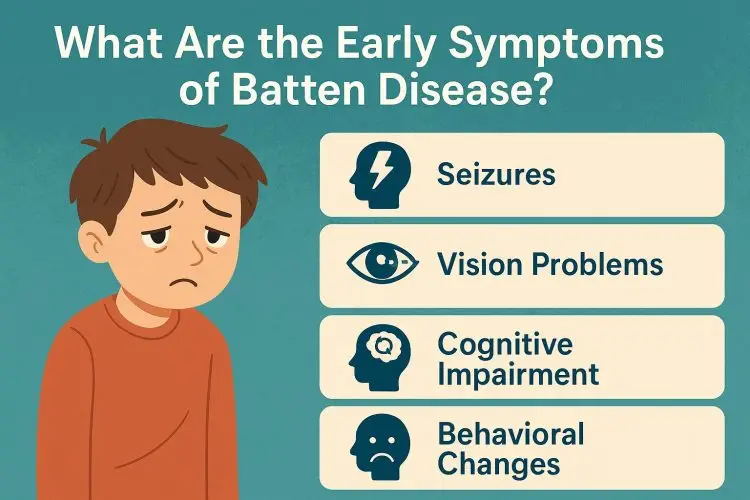
A breakthrough in a diagnostic odyssey often comes from one of two places: the emergence of a “hard” neurological sign that is impossible to ignore, or finding a clinician who is willing to listen and think outside the box. As the disease progresses, the symptoms of something like Batten Disease become more pronounced—the vision loss becomes undeniable, or the seizures become more complex and resistant to standard treatments.
This is also the time when the power of patient advocacy truly ignites. Emboldened by desperation, you learn to push back. You come to appointments with a meticulously organized binder containing a timeline of symptoms, videos of concerning events, and research you’ve done on sites like medicationsdrugs.com. You realize that you have the right, and the responsibility, to be an equal partner in your child’s care.
The Power of Pattern Recognition
The turning point often happens when a doctor—frequently a new specialist at a major academic medical center—takes the time to listen to the entire story from the very beginning. They hear about the early vision problems, the onset of seizures, *and* the subtle cognitive slowing, and they recognize a pattern. They see that these are not three separate issues, but likely three manifestations of a single, underlying systemic disease.
This moment of validation is life-changing. After years of being made to feel like you were imagining things, hearing a doctor say, “I see what you’re seeing, and I agree that something serious is going on,” is a profound relief. It is the first light at the end of a long, dark tunnel.
The Courage to Seek a Second Opinion
If you are not getting this validation, it is crucial to find the courage for seeking a second opinion, or even a third or fourth. This is not a betrayal of your current doctor; it is a responsible act of due diligence for your child. Finding a physician who has experience with very rare neurodegenerative diseases can make all the difference. They are more likely to recognize the subtle patterns and know which advanced diagnostic tests to order.
Trust your gut. If you feel that you are not being heard or that your concerns are not being taken seriously, you have the right to seek care elsewhere. You are your child’s only voice, and you must use it until someone listens.
The Final Chapter: The Journey to a Genetic Diagnosis and Beyond
Once a rare genetic disorder is suspected, the case is usually referred to a clinical geneticist. This specialist is the ultimate medical detective, trained to piece together a family history, clinical symptoms, and advanced testing to find a unifying diagnosis. This is the final leg of the diagnostic journey.
The primary tool at this stage is advanced genetic sequencing. The diagnostic process culminates in a test—often a whole exome or genome sequencing—that can analyze thousands of genes at once to find the specific mutation responsible for the child’s illness.
The Role of the Geneticist and Advanced Testing
The geneticist will take a detailed family history and perform a thorough physical exam, looking for subtle clues. They will then explain the process of genetic testing. Waiting for the results of these tests can be another agonizing period, often lasting several weeks or months. This is a time filled with a strange mixture of dread and a desperate hope for an answer, any answer.
When the results finally come in, the geneticist and a genetic counselor will sit down with the family to explain the findings. Hearing the words—the name of the disease—is a moment that is seared into a parent’s memory forever.
Life After the Odyssey: The Grief and Relief of an Answer
The end of the diagnostic odyssey brings a tidal wave of conflicting emotions. There is the profound, earth-shattering grief of the diagnosis itself and the terrible prognosis that often comes with it. But underneath the grief, there is often a quiet, exhausted sense of relief. The search is over. The uncertainty is gone.
You finally have a name for the enemy you have been fighting. You are no longer an anxious parent; you are the parent of a child with a known, specific disease. This genetic diagnosis unlocks a community of other families, a pathway for care, and a clear direction for your advocacy. The odyssey in the wilderness is over, and a new, different, but clearly defined journey can now begin.
References
For families currently on a diagnostic odyssey, resources from the National Organization for Rare Disorders (NORD), Global Genes, and the Undiagnosed Diseases Network (UDN) can provide support, guidance, and hope. They offer resources on how to be an effective advocate and connect you with others on a similar path.




